

A trailblazing chemist digs deep on resistance to chemotherapy. What he and his team discover may prevent needless chemo treatments, open different treatment pathways and have application to other cancer biomarkers – a gamechanger for oncology, the healthcare system and, most of all, patients.
(View on York University’s website)
Resistance to chemotherapy shortens the life expectancy of cancer patients. The research world has been searching for its predictors for decades, but to date reliable ones exist only for a few cancer types. The problem is in poor reliability of methods. That is what York University Chemistry Professor Sergey Krylov wants the research world to recognize and address.
In collaboration with the Princess Margaret Cancer Centre, Krylov sought to predict chemoresistance in ovarian cancer, which could prevent useless chemotherapy rounds and suggest the use of alternative therapies for chemoresistant patients.
The findings of this research, funded by the Natural Sciences and Engineering Research Council of Canada and discussed in a Perspective published in Analytical Chemistry (2020), could have application to other types of cancer. In short, this could be groundbreaking.

Krylov, who runs an interdisciplinary lab, is focused on creating innovative and enabling technologies for the biomedical world. He sat down with “Brainstorm” to discuss this promising research and its possible impact.

Q: Why is cancer hard to treat and how have we been doing it?
A: First, cancer is not a single disease. There are many types and subtypes that require different treatments. Moreover, patients with the same cancer subtype may respond to therapy differently. Treatment strategy should be defined individually for every patient. This is what is called precision oncology. It entails a set of diagnostic tools that allows us to choose a drug or treatment that is most suitable for each patient. Unfortunately, precision oncology is not here yet. We still use the one-size-fits-all approach.
Cytotoxic chemotherapy, which kills cancer cells because they divide fast, is the oldest treatment (after surgical removal). Unfortunately, chemotherapy also kills fast-dividing normal cells causing devastating side effects, and in many cases, it simply does not work due to tumor chemoresistance.
Q: You sought to better predict chemoresistance. Why is predicting so important?
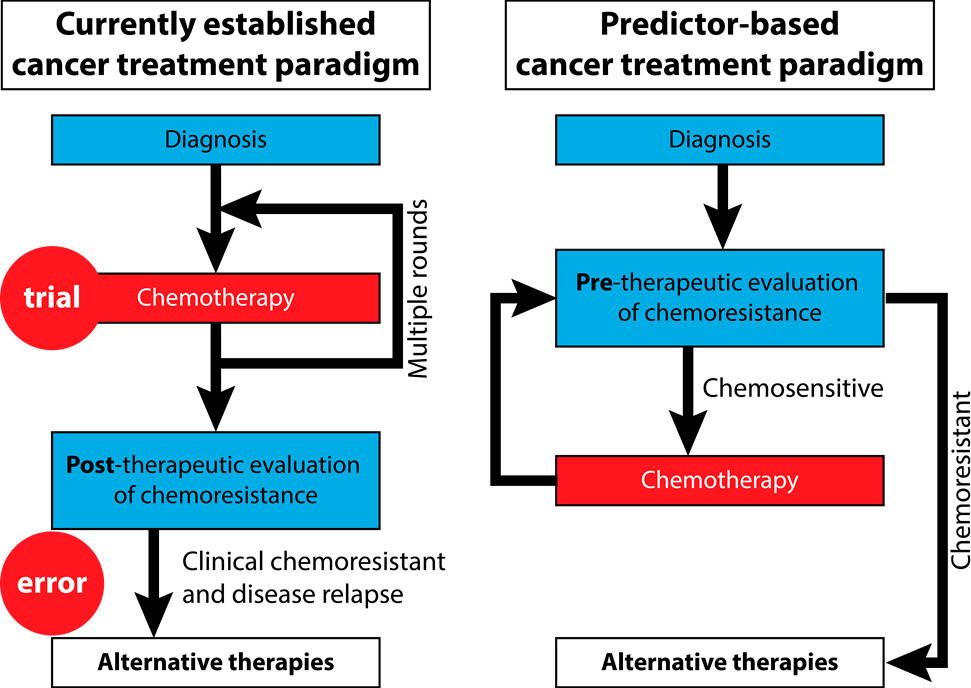
A: Chemotherapy is the first-line treatment for many cancers, and in the absence of a chemoresistance predictor, it is applied by default frontline for every patient. We use a trial-and-error approach: If the patient is chemoresistant, we will know this after months of useless and devastating chemotherapy by seeing that the tumor did not shrink.
The situation would be completely different if we had predictors. There are alternative therapies, which may be less effective overall, but they should be used instead of chemotherapy in chemoresistant patients.
If you do not predict, you expose many patients to unnecessary treatment with severe side effects and delay the use of an alternative therapy. This issue of chemoresistance is fundamental. It can save lives, save time and reduce suffering.
Q: Why did you look at ovarian cancer?
A: There are no chemoresistance predictors for ovarian cancer, but they are really needed here. Eighty per cent of ovarian cancer is diagnosed at an advanced stage and all these cases are treated with chemotherapy. Thirty per cent of these women have intrinsic chemoresistance. Even worse, the majority of those for whom the first round of chemotherapy worked well will have cancer recurrence and will be treated with chemotherapy again. This continuing treatment will eventually result in chemoresistance after the second or later round. It would be great to also have predictors of chemoresistance acquired during the chemotherapy treatment.
Q: Could you describe Princess Margaret’s tissue bank, your source?
A: Princess Margaret has been working on ovarian cancer for decades. They have had some 230 patients from whom they extracted tissue samples, froze and kept in a bank. Advantageously, these samples are accompanied by comprehensive clinical history of every patient. We will use these samples for predictor development.
Q: In what way was your research original and what was the key finding?
A: In general, research on predictors began right after chemoresistance was discovered, and that was right after chemotherapy was invented. There have been over one million research papers published on predictive biomarkers of cancer over the last 50 years, billions of dollars and an enormous number of hours spent on this research. But there are only 11 chemoresistance predictors approved by the Food and Drug Administration.
After 50 years of work and a million research papers, the non-effectiveness of global efforts to date is shocking. It means there is a tremendous waste of resources. This is what we’re trying to vocalize as loudly as possible.
Our research is original in the sense that we started realizing and raising awareness that the problem is methodological – that is, the problem is in the tools that we use. Until we have tools that are reliable, we will not be able to develop any reliable biomarkers.
To clarify, we were invited by the journal to write a point-of-view paper, a critical review. It was an important paper for us because it was an opportunity to say what we think.
Q: What is next for this research?
A: Our work is at the early stages. We are just about to start working with the patients’ tissue samples. The practical results are five to ten years away from now.
We are currently writing a CIHR [Canadian Institutes of Health Research] grant application for developing an ovarian cancer chemo resistance predictor. This is in collaboration with Professor Chun Peng at York University, Drs. Laurie Ailles and Geoffrey Liu at Princess Margaret, and Drs. Allan Covens and Jelena Mirkovic from Sunnybrook Research Institute.
Q: Could this finding be applied to various cancers? And what kind of an impact could better predict chemo resistance make for oncology, the healthcare system and patients?
A: Yes, our technology could have application to other cancer types.
The impact would be revolutionary, but it would need to be a collective effort. Many other technology developers should join our effort in search of robust approaches, which would convert into practical tools for the creation of reliable therapy-guiding biomarkers.
I hope I can convince a good group of researchers to join us; I hope to create a little wave, and that the wave would grow, and more and more people would join this effort.
To read the research article, visit the website. To learn more about Krylov, visit his Faculty Profile page.
To learn more about Research & Innovation at York, follow us at @YUResearch; watch our new animated video, which profiles current research strengths and areas of opportunity, such as Artificial Intelligence and Indigenous futurities; and see the snapshot infographic, a glimpse of the year’s successes.
By Megan Mueller, senior manager, Research Communications, Office of the Vice-President Research & Innovation, York University, muellerm@yorku.ca
